If you sell Medicare Advantage plans, it's important to understand how step therapy works.
Your clients deserve to understand this managed care component of their plan, which can be frustrating if they aren't prepared for it.
What is step therapy?
Step therapy requires patients to try less expensive medications first. If the less expensive medications don't work, they can "step up" to more expensive options. Step therapy, a type of prior authorization, is a part of many Medicare Advantage plans.
Original Medicare does not permit step therapy for Part B drugs.
Step therapy is also known as "fail first," because it requires patients to fail on inexpensive medications first before they can get coverage approval for more expensive options.
When did step therapy begin for Medicare Advantage plans?
Medicare Advantage plans were allowed to apply step therapy to their plans starting January 1, 2019 as part of the American Patients First Blueprint.
More specifically, MA plans can use step therapy for physician-administered and other Part B drugs.
How does step therapy work?
If an MA plan member takes a drug that requires step therapy, they'll have to try less expensive options first.
The MA plan will have specific instructions on which medications they must try and fail on before getting approval for the more expensive option.
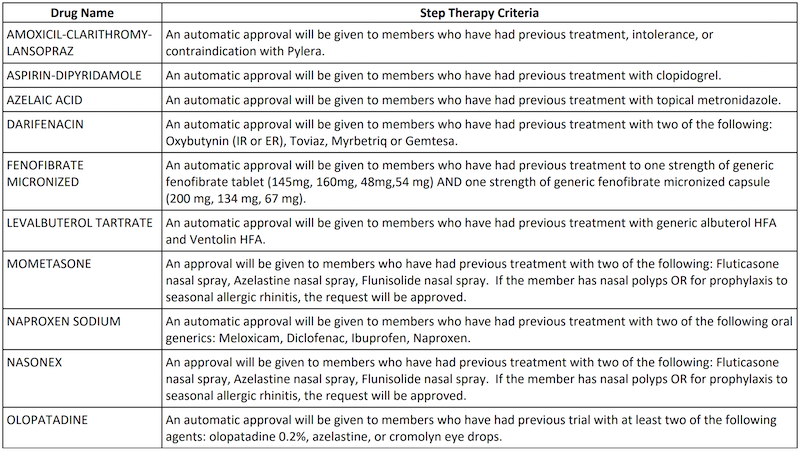
For example, one of Humana's MA plans requires step therapy for the medication azelaic acid. The patient has to try topical metronidazole and fail on it before they can get approval for azelaic acid.
Another example from an Aetna MA plan requires step therapy for several types of Humalog and Lyumjev insulins. The patient must have a documented trial of one month of a Novo insulin or a documented contraindication to Novo Nordisk brand insulins.
Here's a look at some step therapy examples:
Is step therapy bad?
There's a lot of division when it comes to the merits of step therapy. On one side, step therapy helps reduce costs for MA plans and patients. However, patients may spend more time not getting the effective treatment they need.
Those In Favor of Step Therapy
For CMS and other proponents, step therapy helps Medicare Advantage plans negotiate on behalf of beneficiaries to get better value for Part B therapies.
In addition, step therapy helps reduce costs for both the MA plan and the beneficiary.
At first glance, step therapy looks like just another way to save the plan money and line the pockets of private insurance carriers. However, MA plans are required to share more than half the amount saved with the patient as part of the drug management care coordination program.
I personally happen to like step therapy. It was introduced into the group business about 25 years ago, and a lot of people were angry about it. I wouldn't be happy if I had to go through the step program, either, but when 30% of total costs are prescription drug benefits, you have to find a way to contain them. And Medicare is no different.
Plans are simply finding a way to contain costs, which allows them to offer more competitive plans and value to their policyholders.
Those Against Step Therapy
On the other side of the argument, Xcenda, a company that focuses on outcomes research, explains step therapy leads to medication nonadherence, needlessly paying out of pocket for a medication, or stopping medication use altogether.
If an MA plan requires step therapy, a patient may have to take several inexpensive medications – and fail on all of them – before getting approval for a more expensive, specialty drug.
Xcenda argues this leads to higher OOP costs and people spending long periods of time not getting the treatment they need.
Dozens of medical societies and patient advocacy organizations, including the American Medical Association and the American College of Physicians, sent letters to CMS expressing concerns about the consequences of step therapy.
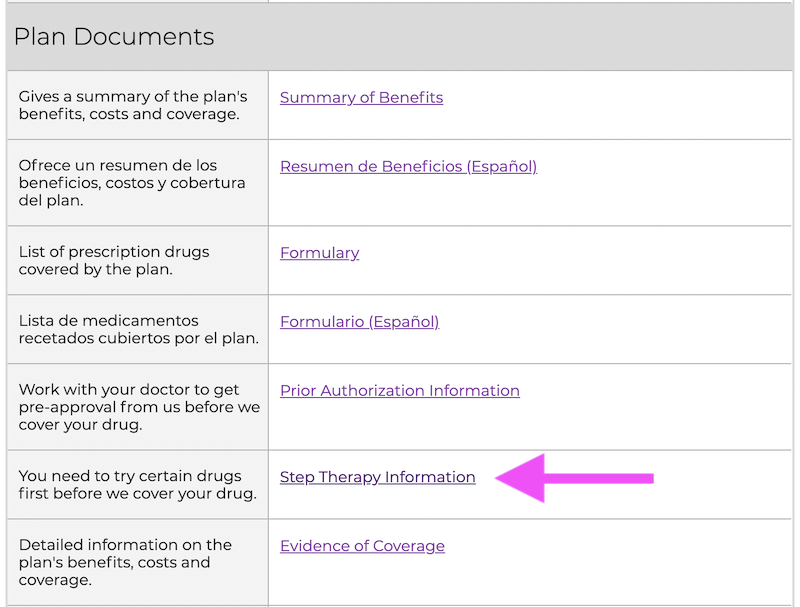
How do I know if a Medicare Advantage plan has step therapy?
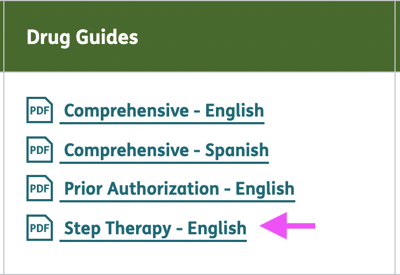
Finding out which medications require step therapy requires a little homework. You have to find the plan's formulary, or a list of covered drugs, and look for the abbreviation "ST." if a drug has "ST" listed next to it, it requires the patient to try cheaper alternatives first.
In most cases, you need to visit the MA plan's website and locate the list of covered drugs.
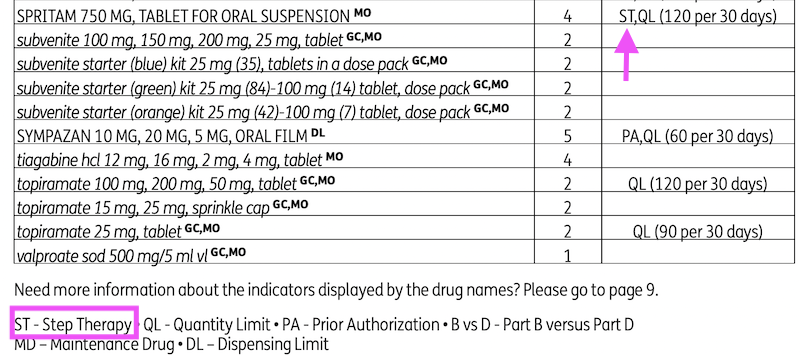
You should also be able to find a special document with step therapy criteria. Here are a few examples of what to look for on the carrier's site:
How can I help my clients with step therapy?
If your client is interested in a Medicare Advantage plan, get a list of their current medications.
When you determine your top plan recommendation for the client, download the list of covered drugs and the step therapy document, if available. Check if any of their current medications require step therapy. If so, inform your client of how step therapy works, and find a new plan recommendation if needed.
At this time, there is no information about step therapy on Medicare.gov's plan finder. Ensure you visit the plan's website, locate the documents you need, and check for step therapy requirements.
Conclusion
Step therapy is incredibly common among Medicare Advantage plans. While it doesn't affect all plans and all medications, it's always best to do some homework to ensure your client is informed.